
by Lara Land | Apr 9, 2023 | COACHING, COMMUNITY, LAND BLOG, LARA LAND, Self Improvement, SELF-IMPROVEMENT
As a society, we are becoming increasingly aware of the impact of trauma on individuals and communities.
Trauma can arise from a wide range of experiences, including abuse, neglect, violence, accidents, natural disasters, and more. For people in the healing professions, including healthcare providers, therapists, counselors, and social workers, it is essential to have a deep understanding of trauma and its effects on patients and clients.
Trauma-sensitive care is an approach that recognizes the prevalence and impact of trauma and seeks to create an environment that promotes healing and safety. Trauma-sensitive care is not just about being aware of trauma; it also involves providing care that is supportive, compassionate, and respectful of the patient’s experiences and needs.
Here are some reasons why folks in the healing professions should have trauma sensitivity training:
- Trauma is common: According to the National Council for Behavioral Health, 70% of adults in the United States have experienced some form of trauma in their lifetime. For people in the healing professions, it is likely that many of their patients or clients have experienced trauma. By having trauma sensitivity training, professionals can better understand the impact of trauma on patients and provide appropriate care.
- Trauma can impact physical and mental health: Trauma can have significant impacts on physical and mental health. It can increase the risk of chronic conditions such as heart disease, diabetes, and obesity. Trauma can also lead to mental health conditions such as depression, anxiety, and post-traumatic stress disorder (PTSD). By understanding the impact of trauma on health, healthcare providers can better support patients and provide appropriate care.
- Trauma can impact trust: Patients who have experienced trauma may have difficulty trusting healthcare providers. They may feel anxious or fearful about medical procedures or may avoid seeking medical care altogether. By having trauma sensitivity training, healthcare providers can create a safe and supportive environment that helps patients feel more comfortable and trusting.
- Trauma sensitivity training can improve patient outcomes: Research shows that trauma-sensitive care can improve patient outcomes. Patients who receive trauma-sensitive care are more likely to stay engaged in treatment, have better physical and mental health outcomes, and report feeling more satisfied with their care.
There are other reasons as well…
- Trauma is pervasive: Trauma is a common experience for many people, and it can have a significant impact on their mental health. Mental health professionals need to be able to recognize the signs and symptoms of trauma, and understand how to provide appropriate treatment.
- Trauma can be complex: Trauma is not always straightforward, and it can manifest in a variety of ways. Trauma sensitivity training can help mental health professionals to develop a nuanced understanding of trauma, and to be better equipped to help their clients.
- Trauma can be retraumatizing: Mental health professionals who are not trained in trauma sensitivity may inadvertently retraumatize their clients by using language or techniques that are insensitive to their experiences. Trauma sensitivity training can help professionals to avoid this.
- Trauma sensitivity is ethical: Providing trauma-informed care is not only beneficial to clients, but it is also an ethical imperative for mental health professionals. Trauma sensitivity training can help professionals to uphold the highest ethical standards in their work.
- Trauma sensitivity is effective: Research has shown that trauma-informed care can be more effective than traditional approaches for clients who have experienced trauma. By seeking trauma sensitivity training, mental health professionals can improve their ability to help clients heal and recover.
In conclusion, having trauma sensitivity training is essential for folks in the healing professions. It helps healthcare providers understand the impact of trauma on patients, provides appropriate care, creates a safe and supportive environment, and improves patient outcomes.
For these reasons and more, I am focusing my Montclair AND Kripalu trauma-informed training on folks in the healing professions including mental health professionals, therapists, psychologists, and others. It is urgent that we are able to heal our own trauma and avoid retraumatizing ourselves and those we seek to help. Learn more about these and my other trainings HERE.

by jimmycrow | Apr 2, 2023 | COACHING, COMMUNITY, LAND BLOG, LARA LAND, Self Improvement, SELF-IMPROVEMENT
Dr. Christiane Wolf is a renowned expert in the field of mindfulness meditation and pain management. Her work focuses on helping individuals use mindfulness practices to reduce physical and emotional pain and improve their overall well-being.
Inexplicable and chronic pain is a common occurrence for trauma survivors especially those who have experienced early childhood trauma.
One of the key insights from Dr. Wolf’s work is that mindfulness can help individuals manage pain more effectively. Mindfulness is the practice of paying attention to the present moment with an attitude of curiosity and openness. By bringing this mindful awareness to physical sensations, individuals can learn to observe their pain without becoming overwhelmed by it. This can help reduce the emotional suffering that often accompanies chronic pain.
Dr. Wolf’s research has shown that mindfulness practices can help individuals reduce their reliance on pain medication. This is particularly important in light of the opioid epidemic, which has highlighted the risks associated with the long-term use of these drugs. By learning to manage pain through mindfulness practices, individuals can reduce their need for medication and avoid the negative side effects associated with long-term use.
Another important insight from Dr. Wolf’s work is that mindfulness can help individuals cope with the emotional challenges of living with chronic pain. Chronic pain can lead to feelings of frustration, anxiety, and depression. Mindfulness practices can help individuals develop the skills they need to manage these emotions and improve their overall quality of life.
Dr. Wolf has emphasized the importance of individualized treatment when it comes to mindfulness and pain management. There is no one-size-fits-all approach to mindfulness, and different individuals may respond better to different practices. By working with each patient to develop a personalized mindfulness plan, Dr. Wolf has been able to help many individuals achieve better pain management and overall well-being.
In the latest episode of the Beyond Trauma podcast Christiane and I discuss different kinds of pain, including transformational pain, how to work with them, and what has worked for each of us. Please take a listen, rate, and review!

by Lara Land | Mar 26, 2023 | COACHING, COMMUNITY, LAND BLOG, LARA LAND, Self Improvement, SELF-IMPROVEMENT
One of the first things folks tend to recognize when they commit to yoga or meditation practice is the incessant internal dialogue going on in their heads.
Our inner voice or really voices have full conversations with each other, make things us, or narrate experiences we already know about.
If we repeated their language out loud, folks would surely think we were nuts.
When we believe everything our inner voices tell us, that is problematic as well.
Learning to understand, not stop, our inner dialogue is what we do in our mindful practices.
Thinking we shouldn’t think is one of the major misconceptions beginner and long-term meditators make. It’s much more about experiencing with awareness the ways thoughts arise and disappear so as understand their nature as well as looking at habits of content on occasion. This is all work I practice with my students on retreats, in workshops, and during private and group lessons.
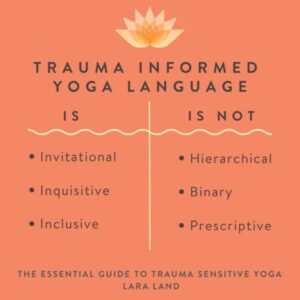
What I want to talk to you TODAY about is how we talk to others which is highly related to how we talk to ourselves, so much so, that adjusting one will often regulate the other.

I want to relay as strongly as possible the difference in experience when the body hears, “You need to…” versus “You might want to try…” OR “You always…” versus “I’ve noticed you tend to…”
Try it now if you like.
These are widely different experiences and they have extremely different repercussions on our nervous systems.
Language is a habit. It develops through what we hear as a child and take in later in life. All habits can be rewired.
This is the bulk of what I teach my trauma informed workshops and trainings. I spoke about it more specifically in this recent VIDEO
The way you experience yourself and others, in other words, your life quality will be drastically improved by even a slight shift in your inner or outer dialogue.
Learn more about how to make this shift in my forthcoming book, The Essential Guide to Trauma Sensitive Yoga: How to Create Safer Spaces for All which is now available for pre-order, or join me for any of my upcoming offerings.

by Lara Land | Mar 19, 2023 | COACHING, COMMUNITY, LAND BLOG, LARA LAND, Self Improvement, SELF-IMPROVEMENT
The war on trans people has been intensifying in recent years, with a wave of anti-trans legislation sweeping across the United States. Many states are passing laws that restrict access to gender-affirming healthcare, including hormone therapy and gender-confirming surgery. These laws can have devastating consequences for trans individuals, who may be unable to access the care they need to live authentically, comfortably, and trauma free.
Gender-affirming therapy, also known as gender-confirming therapy, is a crucial component of healthcare for many transgender individuals. This therapy can take many is designed to help trans individuals align their bodies and identities in a way that feels authentic and comfortable. However, not all trans individuals have access to gender-affirming therapy, and the consequences of this can be severe.
As Dr. Gabor Mate’ so eloquently notes in his best-seller, The Myth of Normal: Trauma, Illness & Healing in a Toxic Culture, humans have an innate need to both live true to their most authentic self and to be accepted for who they are. Failure to experience either authenticity or acceptance results in a traumatic split of the internal system. Maté believes that cultivating authenticity and acceptance can help individuals heal from trauma, overcome addiction, and improve their overall well-being.
One of the most significant consequences of not receiving gender-affirming therapy is this impact on mental health. Trans individuals who are unable to access the care they need may experience depression, anxiety, and other mental health issues. This is due to the distress caused by a misalignment between their gender identity and their physical body which doesn’t allow them full authenticity. It is also due to societal stigma and discrimination. Suicide rates among transgender individuals are alarmingly high. According to the American Foundation for Suicide Prevention, suicide attempts are 14 times higher among transgender individuals compared to the general population. The transgender community also experiences a disproportionately high murder rate compared to cisgender individuals and higher rates of physical violence.
Despite these horrifying statistics, the transgender community continues to be filled with bright, courageous, hopeful individuals daring to live their most authentic lives, heal their trauma, and show us all what it could mean to exist beyond binaries. It is via these relationships and teachings that I have grown to envision and understand what a freer nongendered world could look like for all of us. Jacoby Ballard, author, social justice educator and yoga teacher, has been one of my core teachers of the trans experience and the positive impact queer and trans liberation has on all of us.
Jacoby is deeply forgiving, kind, and a “call in” person who is helping other to learn to forgive through his dharma teachings and way of being. In our conversation on the latest episode of the Beyond Trauma podcast we dive into practices of forgiveness, easing anger, and accepting grief. It’s a powerful conversation and one which taught me what it means to be present, and willing to dare to assume the best in others. I hope you’ll take a listen HERE.

by Lara Land | Mar 13, 2023 | COACHING, COMMUNITY, LAND BLOG, LARA LAND, Self Improvement, SELF-IMPROVEMENT
While I started out investigating trauma from the same viewpoint as many of you, spurned by a single event, attack, or natural disaster, my definition of the kinds of events that could cause trauma has grown steadily year by year. I’ve landed most recently on the potential and likelihood of society as it is, filled with scarcity, conflict, fear, and competition being absolutely enough to leave all of us impacted by trauma. This unnatural and toxic load we all carry in today’s society is making us sick and that must be addressed. Simply asking folks to slow down, nap, rest, etc without the support systems to do so is not only impossible but potentially harmful as the correct social safety nets are not in place to make sure that doesn’t cause more harm.
Living a life in a constant state of stress however low is extremely taxing on our systems. In fact, low levels of ongoing stress hormones may be some of the hardest to identify as being present and therefore not be addressed as causing ongoing health problems. Think of a low but constant buzz and the headache and exhaustion that can cause and you will get a sense of what I mean. Or consider an undetected slow leak that drips and drips and drips.
We must also think about the holding in of emotions so regular in our society. Studies show that repressing and suppressing emotions makes us sicker and can cause disease. And yet society does not provide us with acceptable ways of releasing the stress it imposes. My European husband is red hot embarrassed when I scream which is deemed totally inappropriate in his culture, and it’s not that much more okay in the US. We all need to scream, pound a pillow or throw something now and again. The latest trends of Ax throwing and break everything Rage Rooms as entertainment are proof we are desperate for release. Drumming, dancing, trancing, and yes yelling can help get it out!
So, as we look to lessen the allopathic load we can consider multiple pathways including trauma-focused therapy, such as cognitive-behavioral therapy or eye movement desensitization and reprocessing (EMDR), which can help individuals process and cope with traumatic experiences. Mind-body practices, such as yoga, yoga retreats, meditation, and tai chi, can also be helpful in reducing stress and promoting healing. And…as we keep all these therapies in mind we must also work to make breaks, vacation days, and other destressing opportunities more regular and accepted in our social environment or we will never be able to keep up with the heavy load of living in modern society.
If you are interested in learning simple and highly impactful ways of reducing stress and regulating your nervous system for yourself and others, please join me for a yoga retreat at Kripalu Center for Health June 30th-July 2nd where this will be the main area of focus.

by Lara Land | Mar 6, 2023 | COACHING, COMMUNITY, LAND BLOG, LARA LAND, Self Improvement, SELF-IMPROVEMENT
I’ve been leading trainings in trauma-sensitive yoga since 2014 and one thing which I’ve noticed as my content has evolved is how applicable the information is to any field. It has gotten me to believe that all professions, practices, and sports should have trauma sensitivity training for their leadership. It has been gratifying to see that I’m not the only one who has thought this way. Dr. Jamie Marich, the clinical trauma specialist who wrote Transforming Trauma with Jiu Jitsu had this same idea when she wrote that book and continues to feel so.
We speak, in the latest episode of Beyond Trauma, about the need for trauma-sensitivity training in all fields and specifically how the combination of trauma-sensitivity and the Brazilian Jiu-Jitsu martial art mesh so exceptionally to help trauma survivors.
Many of the aspects of Jiu-Jitsu are similar to those of yoga. Depending on the instructor, there can be a strong focus on breathwork in Jiu-Jitsu just like in yoga. This concentration on the precious link between our inner and outer worlds can be both triggering and healing and which way that goes largely depends on whether the Jiu-Jitsu or yoga teacher has trauma sensitivity training.
Similar to yoga, in Jiu-Jitsu, we work with the mind and the body. In each moment there are a variety of choices and positions the practitioner could bring the body into. The act of making a choice can be both empowering and terrifying for a trauma survivor. These different shapes may bring up memories and emotions. In a safe environment, meaning one in which the practitioner feels able to take breaks, make adjustments, and share their experience without it being judged or doubted, both yoga and Jiu-Jitsu present the opportunity for a survivor to be with difficult sensations in a healthy and potentially healing way.
The main difference between the two practices is the closeness with which one works with a partner in Jiu-Jitsu. With the exception of specific yoga styles such as Partner Yoga or Acro Yoga, yoga is usually more of a solitary practice within a group setting. The partner activities central to Jiu-Jitsu make it all the more potentially triggering and sensitive for trauma survivors. This component also provides a place for growth and healing as a survivor gets comfortable letting someone get physically close to them.
Working in partnership, Jiu-Jitsu practitioners learn that size is not the determining factor in overwhelming one’s component. This is a powerful teaching, especially for trauma survivors who may have experienced helplessness. Learning to defend oneself and feeling confident in one’s ability to do so regardless of an opponent’s size is something that is hardly describable if you’ve been overpowered and why we believe this practice of Jiu-Jitsu so essential.
Take a listen to this special episode on iTunes, Spotify, or wherever you listen to podcasts and let me know what you think in your reviews and comments!




Recent Comments